The Link Between Sleep Patterns and Depression
Last updated on: December 13, 2021 • Posted in:If you’ve ever struggled—or struggle now—to get a good night’s sleep, you know how frustrating and discouraging it can be. And you’re not alone. If you ask virtually any depressed person about sleep, you will almost certainly hear about distorted and disturbed sleep patterns:
- Among people diagnosed with depression, three out of four struggle with insomnia, while 15 percent report symptoms of hypersomnia (excessive sleepiness during the day, which can occur on its own or with insomnia).
- Nearly 90 percent of people with severe depression struggle with early-morning insomnia.
- Among people who are not depressed, the presence of insomnia indicates a higher risk for depression later in life.[1]
Why are sleep issues so prevalent among people suffering from depression? Sleep studies done with depressed patients have shown that depression changes our sleep architecture. People who are depressed experience an altered sleep cycle, entering REM sleep more quickly and spending less time in sleep stages three and four.[2]
Sleep stages three and four—the stages associated with delta, or slow-wave, brain activity—are often called “priority sleep” because they are so critical to our emotional and physical well-being. Sleep expert Mary O’Brien, MD, explains the power of these two stages in this way:
Many of our body’s repair processes occur during slow- wave sleep. Muscles, bones, and joints heal assorted injuries and micro-traumas. Skin and other connective tissues regenerate or repair themselves largely during Stage 3 sleep. During Stage 4 sleep, the anterior lobe of the pituitary gland synthesizes between 70 percent and 80 percent of our total daily allotment of growth hormone [which] helps us maintain normal muscle mass, strength, endurance, and stamina. Without adequate levels of growth hormone, you feel like a dishrag!
Many neurotransmitters are synthesized in Stage 4 sleep, including acetylcholine, critical for memory and learning, dopamine, vital for staying focused and alert, and serotonin and norepinephrine, essential for well-being. No wonder sleep deprivation feels so miserable. When we spend inadequate amounts of time in deep, slow-wave sleep, we deprive our brain of what it needs to produce normal levels of hormones and neurotransmitters.[3]
The link between sleep patterns and depression is so prevalent that at The Center our team performs a sleep study with most of our incoming patients to help determine just how much their sleep quality has deteriorated. But the data is a tricky business. That’s because it can be difficult to determine whether a person’s sleep issues are symptoms of their depression or whether trouble sleeping has contributed to the rise of depression. It’s a chicken-and-egg kind of dilemma: Does a person’s depression cause sleep disruption, or does lack of sleep cause depression?
The answer is yes, both. What’s more, I have concluded that it doesn’t matter which came first, sleep disturbances or depression. Each fuels the other, creating a vicious downward spiral. The critical issue is to improve sleep quality so that depression levels will improve as well.
I felt so passionately about the power of a good night’s sleep that I helped design a premium mattress, called The Serenity, along with a sleep-inducing supplement, At Ease PM.
Professional Health Tip from Dr. Gregory Jantz…
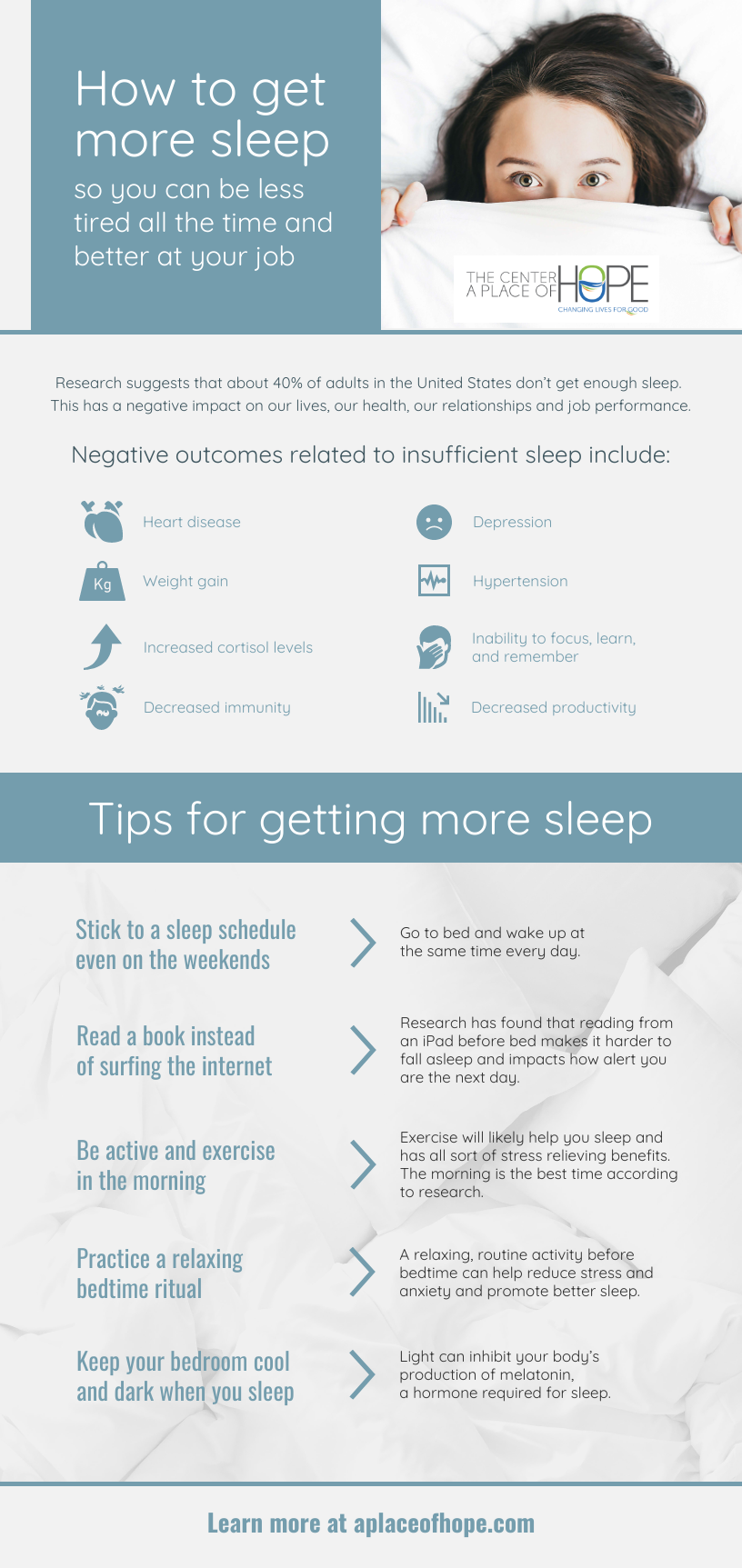
To help improve sleep quality – and help reduce depression – consider these four tips. 1) Invest in a quality mattress. 2) Create a healthy sleep environment that includes darkness, quiet, no blue light, and a cool temperature. 3) Avoid television, heavy meals, and confrontational or difficult conversations within an hour of going to bed. 4) Set a consistent time when you go to bed and maintain that consistency.
Depression and sleep deficits are unarguably entwined. Yet in that interwoven relationship lie opportunities for treatment, relief, and healing. Indeed, when you take measures to improve the quality of a depressed person’s sleep, you also relieve symptoms of his or her depression.
If you are struggling with depression, The Center • A Place of HOPE is here to help. Our team is skilled at navigating these sensitive issues surrounding fear, depression, stress, and anxiety. For more information, fill out this form or call 1-888-747-5592 to speak confidentially with a specialist today.
[1] Harvard Health Publishing, “Insomnia in Later Life,” Harvard Mental Health Letter, December 2006, https://www.health.harvard.edu/newsletter_article/Insomnia_in _later_life.[2] David Nutt, Sue Wilson, and Louise Paterson, “Sleep Disorders as Core Symptoms of Depression,” Dialogues in Clinical Neuroscience 10, no. 3 (September 2008): 329–36, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3181883/.[3] Mary O’Brien, The Healing Power of Sleep (Concord, CA: Biomed Books, 2009), 16–17.Related Posts
What Causes Chemical Imbalance in the Brain? Debunking Myths
By: Dr. Gregory Jantz • Updated: March 17, 2025
Depression isn't just about chemical imbalances—it's more complex. Learn the truth behind the chemical imbalance theory, explore real factors contributing to depression, and find practical steps toward meaningful recovery and lasting mental health.
The Connection Point: How You View Yourself
By: Dr. Gregory Jantz • Updated: October 7, 2018
How you feel about yourself affects all of your other relationships. Some of you may not be used to the idea that you have a distinct relationship with yourself, but you do. You have a personality and a will; you have a perspective on life that is lived out in...
The Effects of Childhood Abandonment in Adulthood
By: Dr. Gregory Jantz • Updated: December 15, 2024
Although there are laws to combat it, childhood abandonment still, unfortunately, happens every day. Childhood abandonment could include instances in which a parent physically abandons or gives up their child, as well as when the child is made to feel abandoned in other ways (such as through loss or neglect).
Get Started Now
"*" indicates required fields
Whole Person Care
The whole person approach to treatment integrates all aspects of a person’s life:
- Emotional well-being
- Physical health
- Spiritual peace
- Relational happiness
- Intellectual growth
- Nutritional vitality